Depression diagnoses have been increasing for years. This article below in 2016 shows the dramatic increases before COVID. Many doctors have been noticing its uptick in our patients, especially during COVID.
Depression can exacerbate the feeling of dry eye symptoms in some patients but so can the medications used to treat depression.
As always, I prefer to try natural options to treat depression. Freud's contemporary psychiatrist and colleague (name coming...) used to say that if everyone went to confession every week which is free, there would be no need for a psychiatrist...even if you are not Catholic. Depression is real, but natural remedies can help. If sleep issues, pain issues, emotional issues can be addressed, we can often get patients off medications for depression.
However, there are many times when a patient does need an antidepressant.
The below study from 2016 ** demonstrated Serotonin-Norepinephrine Reuptake Inhibitor [SNRI] were less likely than Selective Serotonin Reuptake Inhibitor [SSRI] to make dry eye symptoms worse.
Both categories can cause dry eye symptoms to worsen but the general recommendations are below.
SLC
LEAST LIKELY TO MAKE DRY EYES WORSE:
These top 2 were in the below study**.
| Medication | Brand name | FDA Indications | Approval Year | Chemical structure | Notes |
|---|---|---|---|---|---|
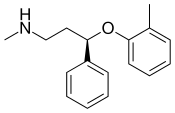
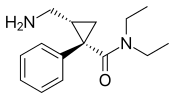
| Atomoxetine[citation needed] | Strattera | 2002 | A norepinephrine-predominant SNRI used in the treatment of ADHD and, off-label, major depression. Was approved by FDA in 2002. Originally considered to be a selective norepinephrine reuptake inhibitor, but research subsequently revealed that it significantly inhibits the reuptake of serotonin at clinical dosages as well.[6] | ||
| Desvenlafaxine[7] | Pristiq Khedezla (ER) |
| 2007 | The active metabolite of venlafaxine. It is believed to work in a similar manner, though some evidence suggests lower response rates compared to venlafaxine and duloxetine. It was introduced by Wyeth in May 2008 and was then the third approved SNRI.[8] | |
| Duloxetine[9] | Cymbalta Irenka |
| 2004 | Approved for the treatment of depression and neuropathic pain in August 2004. Duloxetine is contraindicated in patients with heavy alcohol use or chronic liver disease, as duloxetine can increase the levels of certain liver enzymes that can lead to acute hepatitis or other diseases in certain at risk patients. Currently, the risk of liver damage appears to be only for patients already at risk, unlike the antidepressant nefazodone, which, though rare, can spontaneously cause liver failure in healthy patients.[13] Duloxetine is also approved for major depressive disorder (MDD), generalized anxiety disorder (GAD), diabetic neuropathy, chronic musculoskeletal pain, including chronic osteoarthritis pain and chronic low back pain.[11] Duloxetine also undergoes hepatic metabolism and has been shown to cause inhibition of the hepatic cytochrome P450 enzyme CYP 2D6.[14] Caution should be taking Duloxetine with other medications that are metabolized by CYP 2D6 as this may precipitate a potential drug-drug interaction.[14] | |
| Levomilnacipran | Fetzima |
| 2013 | The levorotating isomer of milnacipran. Under development for the treatment of depression in the United States and Canada, it was approved by the FDA for treatment of MDD in July 2013. | |
| Milnacipran | Ixel Savella Impulsor |
| 1996 | Shown to be significantly effective in the treatment of depression and fibromyalgia.[15] The Food and Drug Administration (FDA) approved milnacipran for treatment of fibromyalgia in the United States of America in January 2009, however it is currently not approved for depression in that country. Milnacipran has been commercially available in Europe and Asia for several years. It was first introduced in France in 1996. | |
| Sibutramine | Meridia | 1997 | An SNRI, which, instead of being developed for the treatment of depression, was widely marketed as an appetite suppressant for weight loss purposes. Sibutramine was the first drug for the treatment of obesity to be approved in 30 years.[17] It has been associated with increased cardiovascular events and strokes and has been withdrawn from the market in several countries and regions including the United States in 2010.[18] | ||
| Tramadol: Dr. Cremers recommend against starting OPIODS as so addictive | Ultram |
| 1977 | A dual weak opioid and SNRI. It was approved by the FDA in 1995, though it has been marketed in Germany since 1977. The drug is used to treat acute and chronic pain. It has shown effectiveness in the treatment of fibromyalgia, though it is not specifically approved for this purpose. The drug is also under investigation as an antidepressant and for the treatment of neuropathic pain. It is related in chemical structure to venlafaxine. Due to being an opioid, there is risk of abuse and addiction, but it does have less abuse potential, respiratory depression, and constipation compared to other opioids (hydrocodone, oxycodone, etc.).[19] | |
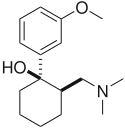
| Venlafaxine | Effexor | 1994 | The first and most commonly used SNRI. It was introduced by Wyeth in 1994. The reuptake effects of venlafaxine are dose-dependent. At low doses (<150 mg/day), it acts only on serotonergic transmission. At moderate doses (>150 mg/day), it acts on serotonergic and noradrenergic systems, whereas at high doses (>300 mg/day), it also affects dopaminergic neurotransmission.[22] At small doses, venlafaxine has also been shown to be effective in treating vasomotor symptoms (hot flashes and night sweats) of menopause and may be as effective as hormone replacement therapy (HRT).[21] |
List Of SSRI Medications
The United States Food and Drug Administration (FDA) has approved the following SSRIs:
Citalopram
Citalopram is prescribed under the brand name Celexa. It’s available as a tablet or liquid.
Although it’s commonly prescribed to treat depression, citalopram can also help treat other mental health conditions, including:
- alcohol use disorder (a disorder that makes you feel unable to control your alcohol use)
- social anxiety disorder (a disorder that causes intense anxiety in social situations)
- panic disorder (a disorder that causes panic attacks, which are sudden episodes of extreme anxiety)
- premenstrual dysphoric disorder (a disorder that causes symptoms like anxiety, irritability, and depression shortly before one’s menstrual period starts)
Escitalopram
Escitalopram is prescribed under the brand name Lexapro. It’s available as a tablet or liquid.
The drug is approved to treat depression in people aged 12 or older. It can also treat generalized anxiety disorder (GAD), which causes frequent, severe anxiety that interferes with daily life.
Fluoxetine
Perhaps the most common SSRI, fluoxetine is prescribed under the brand names Prozac, Rapiflux, Sarafem, and Selfemera. It’s available as a tablet, capsule, or liquid.
The drug is approved to treat the following health conditions:
- depression
- obsessive-compulsive disorder (a disorder that causes recurring, unwanted thoughts and repeated urges to complete certain actions)
- panic attacks
- some eating disorders
- premenstrual dysphoric disorder
Fluoexetine also appears in the drug Symbyax, which is a combination of fluoxetine and an antipsychotic called olanzapine.
Symbyax can treat depression in people who don’t respond well to other antidepressants or who have bipolar I disorder. This disorder causes alternating episodes of depression and mania (a mental state characterized by symptoms like increased energy, euphoria, and irritability).
Fluvoxamine
Fluvoxamine is prescribed under the brand names Luvox (an immediate-release tablet) and Luvox CR (an extended-release capsule).
It’s used to treat depression, obsessive-compulsive disorder, and social anxiety disorder.
Paroxetine
Paroxetine is prescribed under the brand names Paxil, Paxil CR, Pexeva, and Brisdelle. It’s available as a tablet, capsule, or liquid.
Along with depression, paroxetine can help treat:
- panic disorder
- social anxiety disorder
- obsessive-compulsive disorder
- generalized anxiety disorder
- post-traumatic stress disorder
- bipolar disorder
- premenstrual dysphoric disorder
- hot flashes in women experiencing menopause
- chronic headaches
- tingling in the hands and feet caused by diabetes
- sexual problems in men
Sertraline
Sertraline is prescribed under the brand name Zoloft. It’s available as a tablet or liquid.
It’s used to treat the following health conditions:
- depression
- panic attacks
- obsessive-compulsive disorder
- posttraumatic stress disorder
- premenstrual dysphoric disorder
- headaches
- sexual problems
Vilazodone
Vilazodone is prescribed under the brand name Viibryd. It’s available as a tablet.
Currently, the drug has only been approved to treat depression. However, some health care providers also use it to treat anxiety.
Vortioxetine
Vortioxetine is prescribed under the brand names Trintellix and Brintellix. It’s available as a tablet.
Like vilazodone, vortioxetine is only approved to treat depression, but some doctors use it to treat anxiety.
** J Clin Psychopharmacol
Dry Eye Related to Commonly Used New Antidepressants
- PMID: 26075491
- DOI: 10.1097/JCP.0000000000000356
Dry eye patients experience tear film instability with potential damage accompanied by inflammation of the ocular surface.1,3,13,14 This condition is a frequently underrecognized clinical condition and poses strong etiological and management challenges.1,3,7,10 Many studies reported that the DE incidence increased significantly with age and female sex; in subjects with arthritis, Sjögren syndrome, lupus erythematous, ocular rosacea, allergy, and thyroid disease not treated with hormone; in subjects using antihistamines, antianxiety medications, antidepressants, oral steroids, vitamins, β-blockers, and diuretics; and in subjects with poorer self-rated health.7,9,15–17 Depression, hypertension, and benign prostatic hypertension were also associated with an increased risk for DE.2,6,7 Dry eye–related diseases were shown in Table 1. An association between antidepressant use, particularly tricyclic antidepressants and SSRIs, and DE, with decreased lacrimal secretion being the likely mechanism, has been reported in several studies.5–8,16,18 Experimental rat studies suggested that parasympathetic denervation of the human lacrimal gland may induce DE through reduced tear flow and lacrimal protein secretion as well as the activation of inflammatory changes in the gland.19,20 Chronic exposure to histamine and 5-hydroxytryptamine altered the functions thought to be involved in the secretory process, and neuronal release of 5-hydroxytryptamine may be involved in the acute regulation of lacrimal secretion in a broad range of species.19,20
Drugs associated with an increased risk for Dry Eye Symptoms
•β-Blockers
•Diuretics
•Antihistamines
•Anxiolytics
•Neuroleptics
•Anticholinergics
•Parasympatholytics
•Steroids
•Oral contraceptives
•Antiparkinsonian drugs
•Clonidine
•Drugs including pseudoephedrine
Diseases Associated with an Increased Risk for Dry Eye Symptoms:
• Autoimmune Diseases: Rheumatoid Arthritis • Sjögren syndrome • Lupus erythematous • Thyroid disease
• Ocular rosacea
• Allergy
• Depression • Poorer self-rated health • Hypertension • Benign prostatic hypertension
For a first, a very educated patient came in noting that the day he started Wellbutrin and Xiidra on the same day, his stubborn dry eye symptoms of burning, redness, and reflex tearing improved noticeably.
Most often this class of drugs makes dry eye symptoms worse.
But it has been reported that Bupropion (Wellbutrin) to cause excessive sweating. Why does Bupropion do this? Is it due to a change in the brain's internal temperature regulation or a local effect on the sweat glands as noted in below link? Could it help meibomian glands.
Thus far there are no published reports that Bupropion helps dry eye that I could find on a quick literature search. If your eyes have been helped by Bupropion, let us know. jramirez@voeyedr.com
SLC
https://clinicaltrials.gov/ct2/show/NCT01588717
https://www.goodrx.com/blog/medications-cause-excessive-sweating-side-effect/
1) Antidepressants
All classes of antidepressants may cause excessive sweating. Bupropion (Wellbutrin) causes excess sweating in approximately 1 in 5 people
taking it, slightly more often than the typical selective serotonin reuptake inhibitor (SSRI) antidepressants like escitalopram (Lexapro), paroxetine (Paxil), fluvoxamine (Luvox), and sertraline (Zoloft).
Tricyclic antidepressants like amitriptyline (Amitril, Elavil) and nortriptyline (Pamelor) and serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine (Cymbalta) and venlafaxine (Effexor) also cause excess sweating.
Why? SSRIs increase serotonin levels in the brain. Serotonin affects both the hypothalamus, which sets our core temperature at which sweating occurs, and the spinal cord, which may lead to excessive sweating. Tricyclic and SNRI antidepressants cause more norepinephrine to float around the brain, which stimulates receptors (peripheral adrenergic receptors) that lead to sweating.
It is important to keep in mind that sometimes sweating from antidepressants, particularly those involving serotonin, can be a sign of a potentially lethal condition called serotonin syndrome. There is a higher risk if you are taking more than one medication that affects serotonin, or if another medication you take interacts with your antidepressant. Contact your healthcare provider right away if you start experiencing sweating, confusion, muscle spasms, fever, and/or fast heartbeat.
Dry Eye Related to Commonly Used New Antidepressants
- PMID: 26075491
- DOI: 10.1097/JCP.0000000000000356
Abstract
Antidepressants may have an impact on the course of eye dryness. The aim of this study was to investigate the effects of commonly used new antidepressants on eye wetting. Fifty-four patients using new antidepressants and 57 controls were recruited. The Beck Depression Scale and Beck Anxiety Scale questionnaires were completed by the patients, and drug use time and dosages were recorded. The Schirmer test was performed without prior instillation of topical anesthesia to the ocular surface, and the wetting result was recorded for each eye. Escitalopram, duloxetine, and venlafaxine were used by 27, 13, and 14 patients, respectively. The Schirmer test results in the patients were significantly lower than in the controls (P < 0.001). The patients using selective serotonin reuptake inhibitors (SSRIs) displayed lower wetting measurements (≤5 mm) compared with those using serotonin-norepinephrine reuptake inhibitors, which was independent of the duration of antidepressant usage (P < 0.05). Although SSRIs do not have anticholinergic adverse effects except paroxetine, we found that both SSRIs and serotonin-norepinephrine reuptake inhibitors increased the risk for eye dryness. The lower Schirmer test results of the SSRIs may be associated with a mechanism other than the anticholinergic system. An awareness of the drugs that contribute to dry eye will allow ophthalmologists, optometrists, and other physicians to better manage patients who have this problem.
https://www.khanacademy.org/test-prep/mcat/organ-systems/integumentary-system/v/whats-in-sweat-holocrine-apocrine-and-merocrine-glands





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.